In the last few years, we’ve seen demand for telehealth grow exponentially, especially for behavioral health visits. Patients want to talk to their psychiatrist, therapist, or peer support groups without leaving the comfort of their own couches. (And endless supply of tissues.)
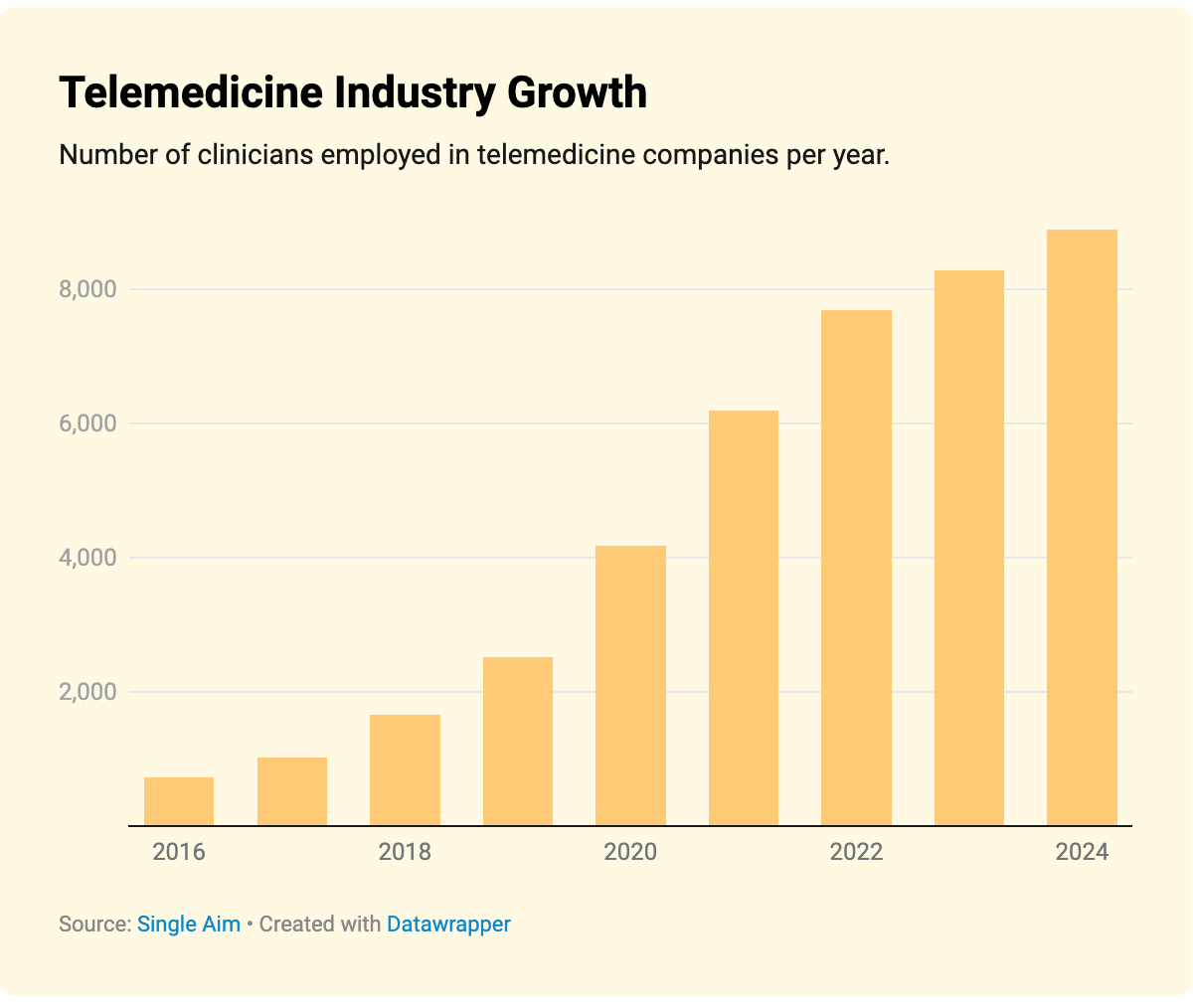
Telemedicine appointments increased by 154% from 2020-2022. This kind of rapid growth for telehealth companies means what was once an easy-to-manage network of clinicians quickly becomes a tangled web of multi-state or multi-country compliance that’s a headache to keep straight for the 1099 filing season.
Our product director, Wade Warren, sat down with two behavioral health experts: Courtney Knitter, supply chain and workforce manager at Meru Health; and Solome Tibebu, president and founder of Behavioral Health Tech, to talk about how behavioral health leaders are strengthening compliance controls, improving payment integrity, and protecting their organizations from financial and reputational risk.
Watch the full video on demand below or read on for key takeaways from the webinar:
“Behavioral health has become so much more visible,” says Courtney. “Because it’s so much more popular, when something goes wrong, it’s much more in the public eye. Moving to virtual, contractor-heavy models means it’s important to think about compliance year-round, not just when you’re onboarding providers or in January come tax time.”
Compliance is a Big Challenge for Behavioral Health Networks
What makes navigating this complexity with compliance so high-stakes is that it impacts patients, providers, and your organization when things go sideways. “So much innovation has been unlocked with telehealth, and now AI,” says Salome. “But keeping up with this technology means keeping up with everything that can go wrong, in a way that’s massively costly and visible, that impacts real people.”
Some of the biggest challenges with compliance for behavioral health companies include:
- Misclassification. “When we were a smaller company, all of our providers were on as full-time employees,” explains Courtney. “As we’ve grown to a multi-state organization, we transitioned them to 1099 contractors, and it’s important to keep that model for us because it balances consistency and stability. But it does mean we have to make sure we’re doing it right on the back end.”
- Variation in state and international regulations. Providers might be licensed in one state and not another, or licensed in several states, which impacts the care they’re allowed to provide legally, as well as requirements, benefits, state taxes, and other regulations.
- Technology that’s not built for contractors. You might have a solid payroll system for W2 employees, but it can’t handle the nuances of an on-again, off-again contractor relationship with providers. At the same time, though, a traditional vendor system that can handle one-off invoices won’t help you with benefits or 1099 compliance down the line.
“I think often, I hear that companies have policies in place, but that usually means they have a handbook or some folder with cobwebs on it,” says Wade. “The real risk hides where the policies disconnect from the daily systems in place.”
For example, most organizations tend to verify licensing and insurance only during the onboarding process. In 2024, an unlicensed woman at Brightside Health allegedly used her wife’s login to counsel hundreds of patients for two years. And the Department of Justice recently charged a clinic owner in Texas who had billed over $4 million to Medicare under resigned or dead therapists.
These are extreme examples, but they’re just as much a reflection of individual bad actors as they are flaws in a system that’s supposed to protect patients and your organization. And there’s no time of year that comes with more risk than during 1099 season, because the IRS doesn’t care whether you made an honest mistake or an intentional one—you’re still stuck paying hefty fines. “I think people tend to treat taxes as an annual administrative item, but you need to be on top of it year-round,” says Wade. “With technology, we often see this as an IT problem, but the provider experience is really fundamental to the business model, because it creates a cascading series of issues that you’ll have to address sooner or later.”
How to Protect Your Organization from Compliance Risk
Keeping your organization safe starts with your contractor management. “Making sure there are tools that guide providers so we can set them up for success and the quality care that they provide is so important,” says Courtney. “We want to give them what they need so they can focus on their patients.”
At Meru Health, they do most of this up-front with their onboarding process. They make sure to conduct the primary source verification up front, alongside gathering other important documentation and data from the provider, like their W9, background check, and payment information. “I think the turnaround time for bringing providers on can really be shortened, which is so important as companies grow,” she says. “You want those providers trained and seeing patients as soon as possible, so automating the process and maintaining continuous compliance is key.”
With any new provider, you’re going to want to have:
- Identity verification: You should be able to prove who a clinician is, including a remote ID capture and selfie-matching at onboarding, especially with AI becoming more sophisticated at impersonating people in photos and videos.
- Device binding: If a login comes in from a new device, or a new country, the system should flag it and escalate it for review.
- Continuous primary source licensing: To make sure you’re always in compliance, you should be screening against state and federal lists every month, and when there is a hit, it should immediately freeze that provider from continuing to work or receive payments.
- Payment integrity: No provider can see 1000 patients in a single day. You need a system that can use automated logic to flag any kind of suspicious or high-risk activity.
- Directory hygiene: “Regulators are cracking down on ghost networks,” advises Wade. “You need accurate, up-to-date rosters that don’t rely on manual updates.”
- Year-round tax workflow: To make sure you’re ready for 1099 season, you need digital W9s, real-time TIN matching at onboarding, and logic that triggers a 24% backup withholding when the IRS requires it.
- Audit trails: Any time a regulator comes knocking, you need to be ready. Any platform you use for your telehealth providers should be able to export a complete dossier by provider with identity, license, exclusion results, and payment history.”
Much of this protection comes from using the right systems for your team. Says Wade, “It’s an overall system architecture question, because companies often have to pull together several different tools to build this workflow. Most organizations keep payments, identity, and credentials in different silos, but integrating them reduces your overall risk and reduces that administrative burden on your team.”
Design a Compliance Process That Works With Your Clinical Team
With all of these checkpoints, though, you need to make sure you’re considering the provider experience. “I often hear concerns from people that if you turn on this compliance infrastructure, clinicians will revolt,” says Wade. “But personally, I think strong controls can coexist with a good provider experience, if you treat compliance like a product problem.”
What that means is thinking about the provider experience the same way you would your pricing model or conversion funnel: Balancing the amount of friction and ease throughout the entire process so that it feels easy, even when you’re asking them to do something beyond their clinical work. Think of your compliance controls more as guardrails than obstacles. Instead of a separate compliance portal, for example, Wade recommends building the controls into the tools they’re already using.
“One way to do this is to put a heavy lift moment when providers already expect friction, like during onboarding or when they’re already changing their information,” says Wade. “You don’t want to do this five minutes before a session. So front load these checks and only interrupt when something actually changes.”
The second piece of this comes back to how integrated your back-end technology is. “When your information is distributed across a lot of different systems, that’s a big challenge for providers, even if they’re not trying to log in to all of them,” he adds. “The frustration I often hear is, ‘You’re making me type the same thing over and over.’ Good systems talk to one another so those facts are re-used across workflows and auto-populated.”
Finally, show them how compliance benefits them by emphasizing that doing the paperwork helps them get paid easier and faster. “It’s not just for us as a company, but it improves their day to day as well,” says Courtney. “As your network grows, it’s about making sure that teams are connected and people aren’t working in silos anymore. As an example, investing in these pre-built, automated workflows that help us reduce risk frees clinicians up to work across state lines without having to worry about anything.”
How to Get Started With Managing Compliance More Effectively
Compliance can feel like a big, tricky topic, but it really comes down to two things: Your policies and your systems that enforce those policies.
“Companies should definitely be thinking about this, and not pushing it down the line,” advises Courtney.
If you’re looking for concrete actions to get started with this process, start with:
- Audit your 1099 network and identify any gaps in your compliance. This could be your licensing workflows, credentialing workflows, network misclassification, and employee controls. Then, document any gaps you find and take corrective steps.
- Go step-by-step through what it would take to pull a dossier on a single provider, ideally a high-risk one like one that practices in multiple states or deals with high volume. Can you pull their identity, licenses, evidence, exclusions, income, and tax ID easily? Or are you hunting in six different systems? “That will tell you a lot about your current state of compliance,” says Wade. “I think that gives leaders a good sense of where these challenges might emerge in an audit.”
- If you haven’t already, standardize and automate any high-risk compliance processes, whether they’re built directly into your existing workflow and systems or you’ll need to add them in. “These can keep you ready and prepared so you’re not blindsided later on,” says Courntey. “Even a simple dashboard or an automated reminder can make a huge difference in reducing that risk.”
Automating and standardizing your compliance processes is easy with the right tools. Take your 1099 filing process.
With Wingspan, January doesn’t have to be so stressful. Our tools are designed to handle every aspect of contractor management, from payments to tax filing by:
- Implementing real-time W9 collection and TIN verification: Automatically request W-9s and cross-check TINs with the IRS database.
- Creating 1099-NEC forms with one click: Auto-calculate payment totals from past transactions, integrated with financial tools to pull imported payments data.
- Filing and delivering 1099-NEC forms: Once your 1099-NEC forms are ready, Wingspan delivers them directly to contractors and e-files the documents with the IRS and state agencies.
See how Wingspan can streamline your 1099 filing process >


.jpg)